Digital Identity
,
Healthcare
,
Industry Specific
Bipartisan ‘Match IT Act’ Aims to Reduce Risk of Medical Mistakes, Privacy Mishaps

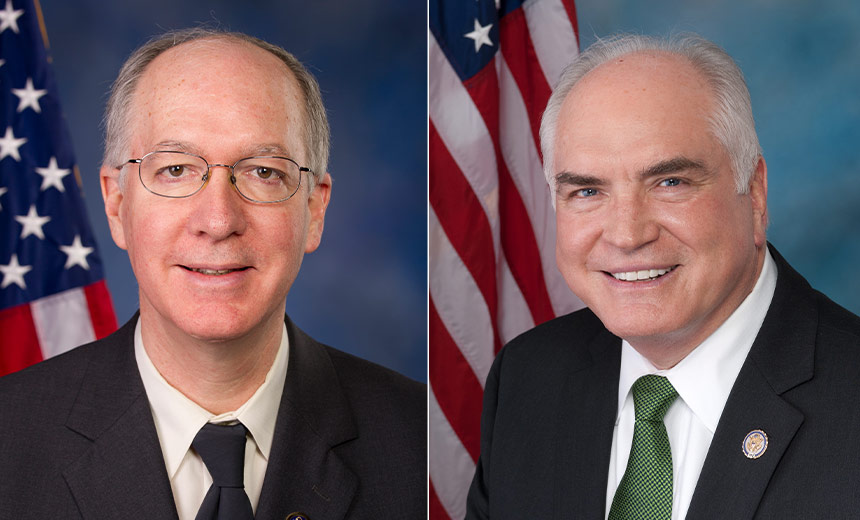
Two Congressmen are taking another bipartisan stab at trying to pass legislation aimed at improving patient identity matching to help reduce mistakes that put patient privacy and safety at risk. The two lawmakers – Rep. Mike Kelly, R-Pa., and Bill Foster, D-Ill., have reintroduced the Patient Matching and Transparency in Certified Health IT Act of 2025 – or MATCH IT.
See Also: Enterprise Browser Supporting Healthcare, Cyber Resilience
The pair in February 2024 introduced an earlier version of the same bill – the MATCH IT Act or 2024. The House Ways and Means Committee – of which Kelly is a member – referred the bill to the House subcommittee on health in December, which was the proposed legislation’s last action before 118th Congress wrapped up (see: Bill Proposes Measuring Accuracy of Patient Matching).
Mistakes in patient matching are costly and deadly – not to mention serious threats to patient privacy, the lawmakers said. Many healthcare experts agree.
More than two dozen healthcare industry groups – ranging from IT professional organizations to medical institutions – said they support the MATCH IT Act of 2025, according the lawmakers.
“Patient matching is a critical problem,” said Terri Ripley, CIO of OrthoVirginia, an orthopedic practice with 160 specialists in 35 locations in Virginia, and one of the entities supporting the bill.
“Health systems have patients coming into the door and registration staff do not find the patient in the system so they create a new patient, we have patients scheduling their own appointments online and putting in data inconsistently,” she told Information Security Media Group.
The expense of repeated medical care due to duplicate records costs an average of $1,950 per patient inpatient stay, and more than $1,700 per emergency department visit, according to a 2021 report by research firm Black Book Research.
In addition, about 35% of denied claims are rooted in inaccurate patient identification, costing the average hospital $2.5 million and the U.S., healthcare system more than $6.7 billion annually, the report said.
In addition to the two MATCH IT Act bills Foster and Kelly have sponsored, they also previously jointly introduced budget amendments to lift a 25-year-old funding ban on the U.S. Department of Health and Human Services that prohibits it from developing or promulgating a unique national patient identification system. That budget provision – Section 510 of the Labor-HHS Appropriations bill – was first enacted by Congress in 1999, and has been renewed annually since then.
The House has previously passed the Kelly-Foster budget amendments related to lifting the HHS ban related to work on unique patient identifiers, but the provisions were either not included or failed to pass the Senate (see: House Again Votes to Lift National Patient ID Ban).
When HIPAA was enacted in 1996, it required the creation of patient identifiers and other uniform standards for electronic data transmission to improve the reliability of health information. But because of privacy concerns, Congress dropped that requirement and instead has repeatedly restricted HHS from working on unique identifiers.
ID Mismatching Risks
Mismatched patient records – such as clinicians or others inadvertently entering or accessing information for the wrong patient, such as an individual with a similar name – has been a longstanding problem in the U.S., leading to medical errors and deaths – as well as billing and other clerical mistakes, experts said.
The Emergency Care Research Institute – ECRI – over the years has listed patient identification errors among the top 10 patient safety concerns for healthcare organizations.
“Healthcare organizations now have the ability to securely exchange patient data, which should be improving the patient’s medical history, but for this to happen we must have patient matching to get the right clinical data to the right patient,” Ripley said.
“High-quality patient care depends on a complete medical history for patients – having patient previous X-rays, surgical history and active medication is critical to caring for patients,” she said.
The MATCH IT Act of 2025 calls for the secretary of HHS, in consultation with healthcare providers, electronic health records and health IT vendors, patient groups and other stakeholders, to “develop a definition and standards for accurate and precise patient matching to track patient match rates and document improvements of patient matching over time.”
“This bipartisan legislation works to improve interoperability between healthcare systems and decrease these fixable matching errors, all while protecting patient privacy,” Kelly said in a statement about the proposal. The bill aims to promote interoperability of patient matching systems “to reduce instances of patient misidentification that cause thousands of unnecessary deaths every year in the U.S.,” Foster said.
Certainly, issues involved with improving patient ID matching have been bouncing around government and the healthcare sector for many years.
In 2019, the Government Accountability Office presented to Congress a study on patient record matching that GAO was mandated to conduct under the 21st Century Cures Act signed into law in 2016. The Cures Act, which focused on advancing medical innovation, contained various provisions aimed at improving the secure exchange of health information for better collaboration among healthcare providers to improve patient care and outcomes.
Among GAO’s report findings, the watchdog agency recommended implementing common standards for recording demographic data (see: Patient Record Matching: Fixing What’s Broken).
HHS’ Office of the National Coordinator for Health IT – which the Biden administration renamed the HHS Assistant Secretary for Technology Policy in 2024 – over the years has attempted to help address patient record matching issues without actually violating the ban on HHS developing an unique patient identifier.
That included the health IT agency taking some measures reflecting GAO’s report findings – including hosting competitions for industry participants to create an algorithm that accurately matched patient records.
The MATCH IT Act of 2025 calls upon ONC – now ASTP – to help further evolve improved patient ID matching. That includes incorporating “a minimum data set for patient matching” as a certification requirement for health IT.
“The MATCH IT Act would improve patient matching without the creation of a patient identifier,” said Cassie Ballard, director of congressional affairs at the College of Healthcare Information Management Executives, a professional association of healthcare CISOs and CIOs, which supports the legislation.
“The bill defines what a patient match rate is, as there is no consistent industry definition for it, and establishes an industry data set to improve patient matching that would be included in the health IT certification program,” she said.
“The primary risk to patient misidentification is patient safety – missed allergies, being prescribed the wrong medication, and delayed or lost diagnoses,” she said. “There are also privacy concerns when patient records are merged – known as overlayed records – and financial implications due to repeated medical care,” she said.
Neither Kelly nor Foster’s offices immediately responded to ISMG’s requests for comment on the MATCH IT Act, including their predictions about whether the bill will gain traction in the current House and Senate.
Overcoming Political Obstacles
In the meantime, some other industry groups, including the Healthcare Information and Management Systems Society, which supports the MATCH IT Act, express optimism that the bill will move forward despite political challenges.
“For many years, HIMSS and our partners on the Patient ID Now Coalition have educated lawmakers about the challenges to patient identification, and we have seen great progress in the House of Representatives where they have removed Section 510 from the Labor-HHS Appropriations bill multiple times,” said David Gray, director of government relations at HIMSS.
“However, making significant changes in legislation, particularly in sometimes politically charged bills like the Labor-HHS Appropriations bill, has proven to be an uphill battle,” he said.
“Congress traditionally defaults to the status quo, which often means leaving in longstanding legacy policy riders. We’ve achieved traction in the Senate, and we will keep pushing in both chambers, but we must continue our advocacy efforts to educate lawmakers about the downstream impacts Section 510 has had and will continue to have until it’s repealed.”
Cyber Considerations
Meanwhile, from a cybersecurity perspective, the conversation about patient ID matching must extend beyond whether to implement a national identifier, some experts said.
“While a national patient identifier could improve care coordination and reduce fraud, it also presents a massive target for cyberthreats,” said Russell Teague, CISO of security firm Fortified Health.
“The healthcare industry must think beyond a single solution and evaluate multiple identity strategies to balance accuracy, security and privacy,” he said.
That includes consideration of emerging AI-driven and decentralized identity solutions, he said. “AI-powered matching algorithms can reduce misidentification rates by detecting patterns and inconsistencies missed by traditional methods, while decentralized identity models – leveraging blockchain or self-sovereign identity principles – empower patients to control their own healthcare data securely.”
